Sleep is a periodic state necessary for the maintenance of the body's vital functions, characterised by a decrease in wakefulness and a cessation or significant weakening of communication with the outside world. Sleep is heterogeneous in structure, and is a complex cyclical process with alternating phases of slow and fast sleep. A total of 4-6 such cycles are recorded during the night. Slow sleep is characterised by a slowdown or increase in the power of electrical waves on the EEG (which directly correlate with sleep depth: the appearance of carotid spindles when falling asleep, the predominance of delta waves when falling into slow sleep) and a decrease in the activity of other physiological functions. During this period, the energy needs of the brain are reduced the most, conditions are created for increased anabolic processes, and protein synthesis is accelerated. During REM sleep (paradoxical phase), there is a desynchronized regular low-amplitude, high-frequency EEG rhythm accompanied by rapid eyeball movement (REM sleep is another name for rapid eye movement). Paradoxical sleep is still a mystery to researchers; its biological significance has not been deciphered, its molecular mechanisms and main functions are unknown. It is hypothesised that it is during this sleep phase that gene expression of chaperone receptors, responsible for proper stacking and configuration of protein complexes synthesised during the slow phase, thereby implementing a protective function preventing brain damage by abnormal protein complexes. Slow-wave sleep predominates in the first half of the night and lasts 60-90 min in the first phase, gradually decreasing closer to awakening, whereas the duration of REM sleep, in contrast, gradually increases from 5 min in the beginning to 30 min by the time of awakening.

A change in sleep patterns occurs with age, in the form of a decrease in slow-wave sleep time and an increase in nocturnal awakenings, from 5% at age 20 to more than 20% at age 85. The average human sleep duration ranges between 6 and 9 hours. However, there are cases in which this parameter falls outside this range, without being accompanied by the disorders characteristic of sleep disorders.
Definition and classification of sleep disorders
The International Classification of Sleep Disorders, Revision 3, 2014 (ICSD-3) defines insomnia as a clinical syndrome characterised by complaints of nighttime sleep disorders (difficulty initiating, maintaining sleep and/or waking early) and associated disturbances during the daytime wakefulness, even though there is sufficient time for sleep and conditions are satisfactory.
The prevalence of insomnia in the general population is 5.7-19%. Transient symptoms of sleep disturbance occur in 30-35% of people. Insomnia is 1.5 times more common in women, and its incidence increases by 10% every 10 years with age, reaching 32.4% at the age of 60-94.
Nocturnal sleep disorders are traditionally divided into pre-, intra- and post-somniac disorders. Presomniac disorders are manifested by prolongation of bedtime, normally the period from going to bed until a full night's sleep does not exceed 30 minutes, with insomnia it may last up to 1.5-2 hours or more. Intrasomnias are characterised by awakening in the middle of the night, with difficulty falling asleep afterwards, lasting 30 min or longer. Postsomnias are characterised by early morning awakenings (at least 30 min before the expected time) followed by difficulty falling asleep. Presomniac sleep disorders are the most common (65%), other variants are less common, and it is not uncommon to have a combination of several types of sleep disturbance. In insomnia, the total duration of sleep is less than 6.5 hours. This is an average value and should not always be used as a basis for a diagnosis of insomnia. For example, the ICD-10 notes that changes in a person's sleep patterns must be taken into account, as there are people who sleep 4-5 hours and do not complain of insomnia; some patients may suffer from poor sleep quality but no change in total sleep duration.
ICSD-3 and ICD-11 divide insomnia into chronic, intermittent and unspecified according to its duration. Chronic insomnia is a sleep disturbance lasting more than 3 months. Chronic insomnia is comorbid with psychiatric and somatic pathology, with approximately 50% of patients with this disorder having a psychiatric disorder. Short-term insomnia is characterised by a duration of up to 3 months and includes acute - transient insomnia and adaptive insomnia. A major role in transient insomnia is attributed to psychological factors associated with emotional overstimulation that disrupts sleep (such as falling in love, arguments, upcoming diagnostic tests for serious illness, etc.); adaptive insomnia also occurs as a result of some kind of emotional distress, usually longer (associated with moving, unemployment, having a chronic somatic illness, etc.). Unspecified insomnia is a provisional diagnosis when a variant of insomnia is established. ICSD-3 identifies short sleepers and those who spend excessive amounts of time in bed as isolated symptoms and separate variants of the norm.
The current ICD-10 does not classify insomnia according to duration, defining insomnia as a sleep disorder (in the form of unsatisfactory duration or quality of sleep) that occurs at least 3 times per week and lasts for at least 1 month. Acute insomnia lasting from a few nights to a week is not considered a nosological entity, because transient sleep disturbance is a normal part of daily life. It is directly related to positive or negative life events that are stressful for the person (e.g. falling in love, serious illness, news of a loved one's disadvantage) and, in the presence of other expressed life-disrupting symptoms (fear, anxiety, depression, inner tension, etc.), can be coded as acute stress reaction (F 43.0) or adaptation disorder (F43.20) in ICD-10.
While short-term insomnia is a stress response of hyperactivation to shocks that have occurred and may go away with favourable resolution or acceptance of the latter, chronic insomnia is a more complex and persistent pathological process that involves various psychopathological factors in its formation. Until recently, several clinical subtypes of chronic insomnia were distinguished, which are reflected in ICSD-2 and are still relevant today.
The psychophysiological type of insomnia is characterised by an excessive fixation on sleep problems, with which the patient associates all subsequent possible disturbances during the day; patients fear the onset of night, their bed, which is associated with insomnia and an uncomfortable state. Due to the increased internal tension of these experiences, they are unable to fall asleep at night and become even more frightened - a vicious circle is triggered (similar to expectant neurosis - the person anticipates failure, imagining a picture of failure, and when the anticipated situation occurs due to nervous overexertion, the anticipated problem actually occurs). Idiopathic insomnia - insomnia has been present throughout the person's life, starting at an early age or since school. Paradoxical insomnia (sleep agnosia) - the degree to which the patient's complaints are inconsistent with actual sleep disturbances, objectification reveals at least a 50% discrepancy between objective findings and subjectively perceived sensations. Insomnia in mental disorders is a consequence of a mental illness, occurs with the manifestation of the latter and worsens with the progression of the illness. ICD-10 considers these variants of insomnia under the heading "Inorganic insomnia F51.0 (mental disorders)". It is noted that if a patient has a psychiatric disorder, insomnia should be coded separately only if it is primary, more prolonged than the underlying disorder, and the patient clearly indicates the dominance of insomnia over other disorders (anxiety, depression, compulsions, etc.), or if it is severe and plays an important role in the clinical picture, making it necessary to treat this condition specifically.
Insomnia with poor sleep hygiene is most common in adolescents and older people due to irregular bedtimes, sleeping during the day, taking stimulants in the evening: coffee, energy drinks, nicotine, alcohol, physical and mental strain shortly before intended sleep. Sleep improves when the unfavourable factors are eliminated.
The ICD-10 separately identifies sleep disturbances in children and adolescents due to untimely putting down, which is regarded as inadequate parental action. This disorder is coded under Z62.0 - inadequate parental care and control.
Insomnia in diseases of the internal organs. These are so-called organic variants of insomnia resulting from a somatic/neurological illness. However, it is often difficult to determine whether the condition is a psychogenic personality response to the presence of a somatic disease (nosogenia) that is prevalent in organic pathology and should be referred to the above-described non-organic insomnia (F51.0). The diagnosis of true organic insomnia can be made with a high degree of certainty when the cause of insomnia is night pain, gastroesophageal reflux, frequent urge to urinate, etc. In the ICD-10, organic insomnia is coded under the heading "Sleep and sleep disturbance (G47.0)". They should be classified as a separate nosological entity only when they significantly affect the patient's well-being and determine additional therapeutic interventions aimed at eliminating the disorder (for example, if insomnia is caused by persistent pain syndrome and this disorder disappears against the background of antinociceptive therapy, then it is not worth making a separate diagnosis; if insomnia is persistent, persists despite success in basic therapy, requires additional therapeutic interventions to eliminate the disorder).
Insomnia with medication and other drugs results from the use of drugs that can have a negative impact on sleep if taken or withdrawn. These include some antidepressants (selective serotonin reuptake inhibitors, clomipramine, venlafaxine, duloxetine), drugs with psychostimulant effects (caffeine, ephedrine, isoniazid, theophylline, interferons etc.). The following are some of the most common drugs: benzodiazepine tranquillisers, sleeping pills, cardiovascular drugs (beta-blockers, statins, alpha-adrenoceptor agonists), hormonal drugs, some antibiotics, etc. Sleep disturbances can occur in the context of a sleep disorder. Sleep disturbances may occur as part of drug withdrawal as well as in withdrawal states. Alcohol intake and withdrawal are also attributed to this variant of insomnia.
Due to the frequent combination of several psychopathological variants of insomnia, the difficulty of classification, and the general approaches to treatment of these conditions, ICSD-3 and ICD-11 do not use this division principle, although virtually all of the above subtypes are taken into account in the diagnosis of insomnia.
Diagnosis of insomnia
An important diagnostic feature of insomnia is the presence of sleep disturbances despite there being no real cause (such as constant noise, bright lights, uncomfortable bed, deliberate limitation of sleep in order to finish homework/work, etc.) - a person has all the conditions for a good night's sleep, but cannot.
In addition to reduced sleep duration, insomnia is characterised by impaired daytime functioning in the form of at least one of the following signs: reduced concentration, memory, daytime sleepiness, irritability, behavioural disorders (impulsivity, aggression etc.), fatigue, general malaise, mood disorders, impaired social communication and family relations, difficulties in work or study, reduced motivation, energy, initiative, susceptibility to mistakes, unhappiness and lack of confidence. The sleep disturbances and daytime symptoms described above should occur in the clinical picture at least three times a week.
For a diagnosis of insomnia, other sleep disturbances must be excluded, which include:
- hypersomnia (manifested by excessive sleep during the day, which can impair the quality of night sleep);
- parasomnias (night terrors and nightmares, hallucinations on falling asleep and waking up, dreaming, sleep paralysis, sleep eating syndrome, bedwetting, etc.)
- (e.g. parasomnias due to medication that can cause nightmares and other disorders);
- breathing disorders (sleep apnoea, caused by obstructive airway changes or respiratory centre pathology);
- movement disorders during sleep (restless leg syndrome, bruxism in sleep, intermittent limb movement syndrome);
- sleep-wake rhythm disorders (early or delayed onset of the sleep phase, irregular sleep-wake rhythm, most often associated with shift work schedules, time zone changes).
The European Society for Sleep Research (2017) recommends that the diagnosis of insomnia and comorbid conditions should include the following indicators:
Somatic examination (mandatory parameter): thorough anamnestic information, if necessary also from carers: past and present somatic diseases (including The patient's somatic condition; and laboratory tests, including general and biochemical blood tests, thyroid hormone levels, C-reactive protein, vitamin B12, and ferritin, if appropriate. EEG, ECG, CT/MRI are performed, and circadian markers such as melatonin and basal body temperature are measured.
Careful collection of psychiatric/psychological history (mandatory parameter): past and/or present psychiatric disorder; personality traits, work and partner relationships; presence of intrapersonal conflict.
Sleep history (mandatory parameter): information about the nature of sleep disturbance, trigger factors; information from the bed partner (sleep apnea, periodic limb movements during sleep; working hours / circadian factors: shift and night work schedule, premature sleep, sleep latency; sleep-wake factors with daytime sleep (keeping a sleep diary, using sleep questionnaires).

Actigraphy - necessarily recommended only when an irregular sleep-wake rhythm or circadian rhythm disorder is suspected.
Polysomnography is necessarily recommended in the following situations: when other sleep disorders such as intermittent limb movement, sleep apnoea or narcolepsy are suspected; in the treatment of therapeutically resistant insomnia; insomnia in the evaluation of patients at risk (for example professional drivers); when there are suspected large discrepancies between the information given by the patient and the actual situation.
Sleep disturbance therapy
Non-medication methods
Insomnia treatment uses a variety of non-medicinal and medicinal methods. The leading role is currently given to psychotherapy, which is due to the large proportion of various psychological aspects involved in the development of this illness. The 3-P model formulated by A. Spielman in 1987 is considered as the mechanism of insomnia formation. Spielman in 1987, according to which in the development of insomnia matter 3 groups of factors: predisposing, provoking and supporting. Predisposing factors include anxious and hypochondriacal personality traits, perfectionism, etc., which contribute to a stronger reaction of an individual to stressful events, making him particularly susceptible to them, with a tendency to form cognitive agitation (the occurrence of anxious thoughts, leading to hyperactivation of the nervous system, preventing normal falling asleep). When a triggering factor (a stressor) interacts with a predisposing factor, insomnia occurs. The more pronounced the predisposing features, the more likely the factors that support insomnia can be formed. The essence of psychotherapy is to remove the dysfunctional connections that have formed and that support insomnia.
Cognitive behavioural therapy (CBT) for insomnia has a high degree of evidence. One option for CBT is behavioural therapy focused on sleep hygiene, which consists of a good sleep-wake routine:
- going to bed and getting up at the same time;
- eliminate daytime sleep, especially in the afternoon;
- avoid the use of stimulants (tea, coffee, nicotine) before going to bed;
- try to avoid stressful situations, reduce mental stress, especially in the evening;
- use moderate physical activity to induce fatigue in the evening, but no later than 3 hours before bedtime;
- Take walks outdoors;
- a cool shower (slight cooling of the body is part of the physiology of falling asleep), in some cases a warm shower causing mild muscle relaxation can also lead to better falling asleep;
- comfortable sleeping conditions: a comfortable mattress, pillow, and a bedroom temperature not exceeding 21°C.
Another variation of CBT is sleep restriction, where bedtimes are reduced to actual sleep time with a gradual increase in this stretch. Stimulus control aims to break down the triggers that sustain insomnia (fear of approaching bedtime, fear of going to bed associated with distressing thoughts of not being able to fall asleep): it is allowed to go to bed only when sleep is desired, if sleep does not come, it is necessary to get up and switch to other activities, eliminate daytime sleep, get up at the same time.
Other non-pharmacological treatments include various relaxation techniques, physiotherapy (transcranial magnetic stimulation, electrosleep, chromotherapy) and balneotherapy (iodobromic baths).
Medication therapy
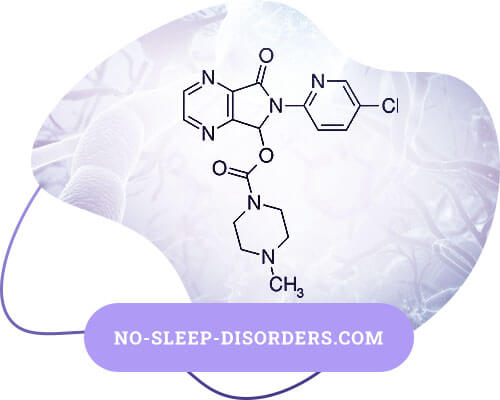
Hypnotics currently being considered are benzodiazepines (nitrazepam, clonazepam, diazepam, lorazepam, temazepam, bromodihydrochlorophenylbenzodiazepine), benzodiazepine receptor agonists (zopiclone, zolpidem, Zaleplon), melatonin, herbal preparations (valerian, peppermint, lemon balm, rogue peony, motherwort), histamine receptor blockers (diphenhydramine, doxylamine).
It should be noted that almost all hypnotics may be addictive, lead to weakening of therapeutic effect, dependence, and often have some or other side effects, so it is recommended that they should be used for short courses, 14-21 days.
There is evidence that 1.5-3% of the population takes sleeping pills regularly and 25-29% occasionally. Abuse of sleeping pills, according to various authors, ranges from 0.2% to 4.5% of the general population.
It should be noted that in general medical practice, in addition to the above hypnotics, physicians have in their arsenal drugs with sedative effects belonging to other classes (antidepressants - trazodone, mirtazapine, mianserine, amitriptyline; neuroleptics - chlorprotixen, alimemazine, quetiapine, promazine, etc.). The drugs (e.g. gabapentin, pregabalin) that, despite their lack of a registered indication for treating insomnia, due to their ability to produce sedative and hypnotic effects are successfully used for the treatment of this condition. An advantage of most of the drugs described above is that there is no risk of dependence and addiction, myorelaxant side effects and ricochet-like insomnia after withdrawal.
The European Guidelines for the Diagnosis and Treatment of Insomnia (2017) recommend CBT as a first-line treatment because of its safety and proven high efficacy; drug treatment is only indicated in cases where it is not feasible. Limitations on the use of certain hypnotics are based on the lack of high-level evidence of efficacy. Benzodiazepines, benzodiazepine receptor agonists and some antidepressants with sedative effects are recommended for short courses of medication. Neuroleptics are not recommended as hypnotics due to unproven efficacy and side-effects, nor are H1-histamine receptor blockers, herbal preparations and melatonin due to unproven efficacy. Pregabalin and gabapentin are considered separately. The same guideline notes that even occasional use of benzodiazepines can increase the risk of mortality.
Most benzodiazepines, benzodiazepine receptor agonists, as well as pregabalin, are classified as controlled drugs requiring special prescription forms, which makes their prescribing very difficult. Benzodiazepines are not recommended for persons over 60 years of age due to their possible amnestic effects and the risk of falls due to myorelaxation. For zopiclone, a 4.3-fold increase in the risk of falls in the elderly has been reported. Thus, of the sleeping pills recommended by the European Guidelines (2017), sedative antidepressants are the most appropriate to prescribe, in addition they are not addictive, addictive, amnestic or myorelaxant.
As an alternative to the above position, based on highly evidence-based research, a number of authors, guided by the ancient "do no harm" principle, recommend starting with herbal medicines and melatonin, citing their safety and good tolerability.
The domestic draft of the Clinical Guidelines for the Treatment of Chronic Insomnia (2016) provides evidence to consider CBT, relaxation, and stimulation control as highly effective, along with benzodiazepine receptor agonists and delayed-release melatonin (the latter was a treatment for insomnia in patients 55 years and older). For other drugs (benzodiazepines, H1-histamine receptor blockers, trazodone, quetiapine, valerian, melatonin), the evidence for their effectiveness is inconsistent, but there are more positive effects, so these drugs can be used to treat insomnia. The authors are of the opinion that the existing restrictions on the time of use of sleeping pills for 2-4 weeks, due to the fear of developing dependence and addiction syndrome, are based on past experience, whereas for modern drugs there is no clinical evidence to support this phenomenon. Studies on the efficacy and safety of hypnotics are short-term and no longer than this time frame is available. Due to the fact that chronic insomnia is a long term disease (recurrence rate can be as high as 70%), there is a debate about the long term use of hypnotics. Interesting data are given regarding individual hypnotics. Melatonin preparations have proven effective in elderly patients, whereas their use at a young age may have adverse effects on fertility. The H1-histamine receptor blocker doxylamine is the drug of choice in pregnant women and has been shown to be effective and safe. Valerian preparations are only effective in high doses, which may cause liver damage. In conclusion, it is noted that neither clinical guidelines nor drug formularies are a substitute for the judgement of the physician based on clinical thinking. The decision on treatment tactics is made by the physician on a case-by-case basis.
Over-the-counter drugs with sedative and/or tranquilising effects (such as phenobarbital-containing drugs, bromcamphor, herbal preparations containing valerian, melissa, mint, motherwort, phabomotisole) are often used to treat sleep disturbances.
The first hypnotics were barbituric acid derivatives, barbiturates, but due to the identified side effects of dependence, addiction, severe withdrawal, neurotoxicity and teratogenic effects, most of them are now discontinued. Phenobarbital, a member of this class, is a controlled substance that is still used as an anticonvulsant backup for the treatment of severe resistant epilepsy. Despite the fact that these drugs are officially considered obsolete (resolution of the RAMS Formulary Committee Presidium meeting of 16.03.2017), they are still actively used by the population, belonging to the category of "folk remedies". The main dangers of their frequent and uncontrolled use are over-sedation, addiction, and the possibility of respiratory depression in overdose (as with benzodiazepines).
Bromine preparations (e.g. Dobrokam®) have the ability to concentrate and intensify inhibition processes in the cerebral cortex through direct action on neurons. According to I.P. Pavlov and his pupils, they can restore the balance between the processes of excitation and inhibition, especially when the CNS is overexcitable. In the past, bromine preparations were used widely enough, including as anticonvulsants. Today, globally recognized balneological procedures - iodobromic baths with proven effectiveness in terms of calming, sedative, anti-stress effect, positively affecting cardiovascular system, peripheral vascular resistance, improving the quality of sleep - retain their relevance. Bromkamfora (Dobrokam®) continues to be used in the treatment of anxiety spectrum disorders including the presence of concomitant cardiovascular pathology. Another component of the drug, camphor, is an analeptic agent that tones up the respiratory and stimulates the vasomotor centre. It has a direct effect on the heart muscle, intensifying metabolic processes and increasing its sensitivity to the action of sympathetic nerves. Under the influence of camphor the peripheral blood vessels are narrowed. Being excreted from the body through the respiratory tract, camphor promotes separation of sputum. There are indications that camphor inhibits platelet aggregation, so it can be recommended for use to improve microcirculation. Camphor solutions are used for complex therapy in acute and chronic heart failure, collapse, respiratory depression in pneumonia and other infectious diseases, in poisoning with sleeping pills and narcotics. One significant disadvantage of benzodiazepines and benzodiazepine receptor agonists is their ability to inhibit breathing, so they are contraindicated in people with respiratory disorders (such as sleep apnoea, etc). The analeptic properties of camphor can be considered an advantage in the therapy of insomnia in patients with cardiovascular and respiratory pathologies. Another advantage is the possibility of using the drug in children from the age of 7 years. An important feature is the development of sedative and hypnotic effects immediately after initiation of administration. Bromkamfora (Dobrokam®) can be considered as a drug of choice for short-term therapy of insomnia, including in presence of concomitant cardiovascular and bronchopulmonary pathology.
Herbal preparations are quite safe to use, but may cause allergic reactions or be insufficiently effective. Fabomotisole is both tranquilizing and stimulant, well tolerated, but with delayed action, so that the expected effects on sleep quality will be gradual.
Conclusion
Diagnosing insomnia requires an in-depth, multidisciplinary, comprehensive examination of the patient, taking into account detailed sleep characteristics, somatic and psychological features. Whenever possible, priority in the therapy of this condition should be given to non-drug methods aimed at eliminating unfavourable factors that interfere with the formation of normal sleep, relaxation. Drug treatment should preferably be of short duration and only when the insomnia significantly affects the ability to function. Due to the lack of an ideal unique hypnotic, universally and effectively effective for all patients suffering from insomnia and completely free of side effects, it is advisable to rely on the individual characteristics of the patient (age, gender, presence of concomitant somatic and/or psychiatric pathology, pregnancy, individual susceptibility, etc.) in choosing a sleeping pill.











